IMPROVE CONTACTABILITY
Connect more effectively with hard-to-reach members
Get a free consultation
Many payers and providers cite missing or outdated phone numbers and contact information as the top challenge when it comes to member engagement, with some payers seeing up to 50% of phone numbers with missing or incorrect information.
Request your free consultation with Prove and Tabula Rasa HealthCare (TRHC) to understand:
![]() How to significantly improve the quality of your existing member contact information and discover additional phone numbers using Prove’s Fonebook™ technology.
How to significantly improve the quality of your existing member contact information and discover additional phone numbers using Prove’s Fonebook™ technology.
![]() How to assess the accuracy of your existing member contact information.
How to assess the accuracy of your existing member contact information.
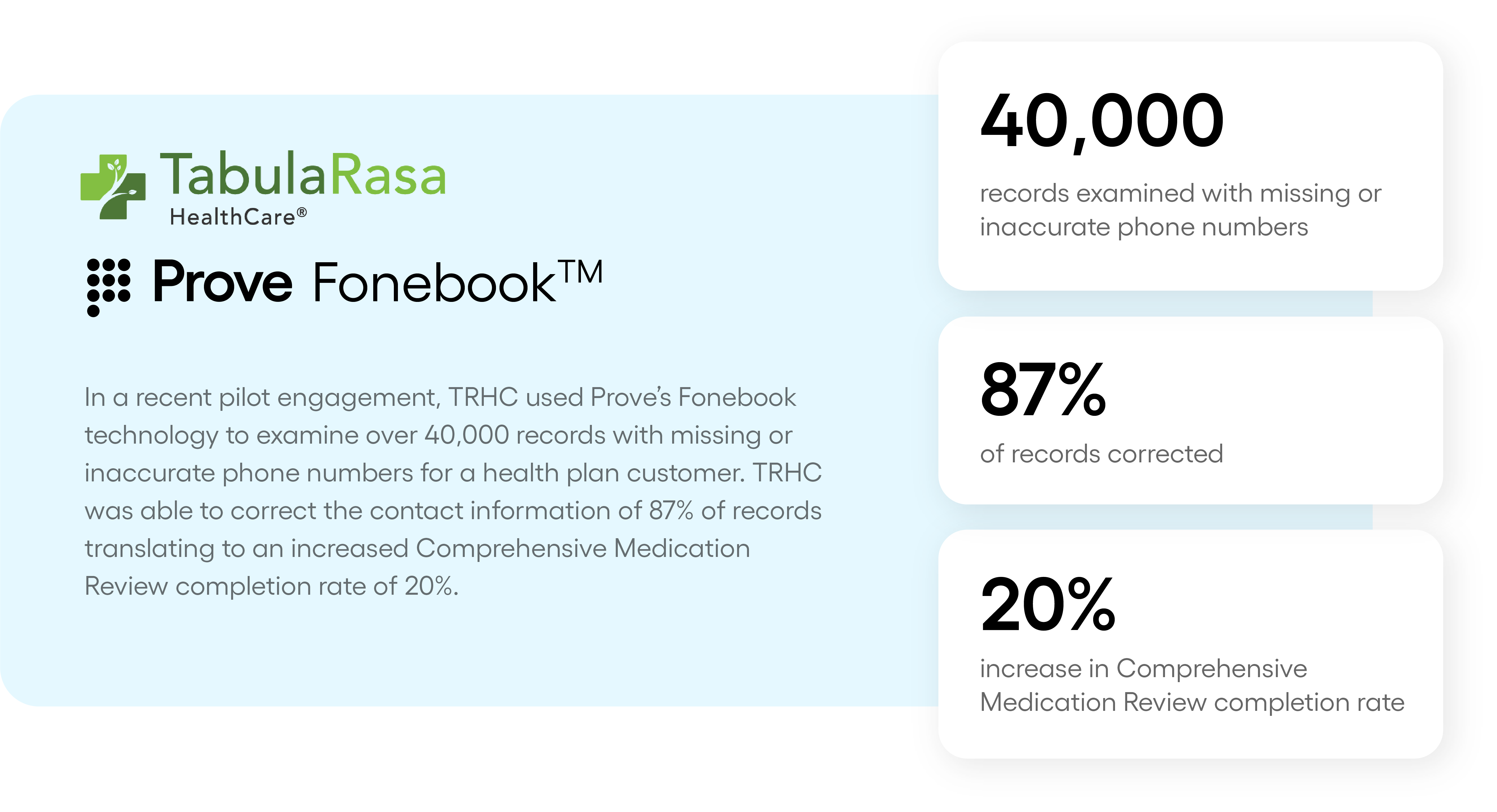
![]() How Prove and TRHC were able to increase one health plan’s correct contact information to 87%, translating to an increased Comprehensive Medication Review completion rate of 20%
How Prove and TRHC were able to increase one health plan’s correct contact information to 87%, translating to an increased Comprehensive Medication Review completion rate of 20%
About Prove
About Tabula Rasa HealthCare
Tabula Rasa HealthCare (TRHC) provides medication safety solutions that empower healthcare professionals and consumers to optimize medication regimens, combatting medication overload and reducing adverse drug events – the fourth leading cause of death in the US. TRHC’s proprietary technology solutions, including MedWise®, improve member outcomes, reduce hospitalizations, and lower healthcare costs. TRHC’s extensive community pharmacy and clinical tele-pharmacy network improves care for members nationwide. Its solutions are trusted by health plans and pharmacies to help drive value-based care. For more information, visit TRHC.com.
Ready to improve your member contactability?
Request more info today to learn how Prove and TRHC can increase your percentage of correct and verified member contact information and help you improve member outcomes.
©2025 Payfone, Inc. DBA Prove. All Rights Reserved. Privacy Policy.